Overview
Caring for an elderly loved one who isn’t eating or drinking can be incredibly challenging. It’s important to first understand the emotional weight this situation carries for both the caregiver and the individual. Many caregivers feel stressed and overwhelmed, often questioning what they can do to help.
To support an elderly person in this situation, there are three essential steps to consider:
-
Start by identifying the reasons behind their appetite loss. This could be linked to medical conditions, medications, or even psychological factors. Understanding these underlying issues can provide clarity and direction.
-
Next, implement strategies to stimulate their appetite. Simple changes, like establishing a routine or enhancing the appeal of meals, can make a significant difference. Think about how you can make mealtime more inviting—perhaps by introducing their favorite dishes or creating a pleasant dining atmosphere.
-
Finally, it’s crucial to monitor their health closely while seeking professional guidance. Regular check-ins with healthcare providers can ensure that any medical concerns are addressed promptly. Remember, you’re not alone in this journey. Many caregivers share similar experiences, and reaching out for support can be incredibly beneficial.
By taking these steps, you can foster better nutritional intake among seniors, helping them feel more nourished and cared for. It’s a journey filled with challenges, but with compassion and understanding, you can make a positive impact on their well-being.
Introduction
Understanding the complexities of appetite loss in the elderly is vital for caregivers who want to ensure their loved ones receive the nutrition they need. It’s heartbreaking to know that nearly 93% of seniors face chronic health issues that can dampen their desire to eat and drink. This challenge weighs heavily on caregivers, who often feel stressed and overwhelmed.
So, what can caregivers do to rekindle interest in meals and encourage healthier eating habits? It’s essential to navigate the emotional landscape of their loved ones’ struggles while finding effective methods to stimulate appetite. Not only does this enhance nutritional intake, but it also significantly improves the overall quality of life for elderly individuals.
By exploring compassionate strategies, caregivers can foster a nurturing environment that promotes better eating habits. Remember, you’re not alone in this journey; there are ways to bring joy back to mealtime and support your loved ones in feeling their best.
Identify Reasons for Appetite Loss in the Elderly
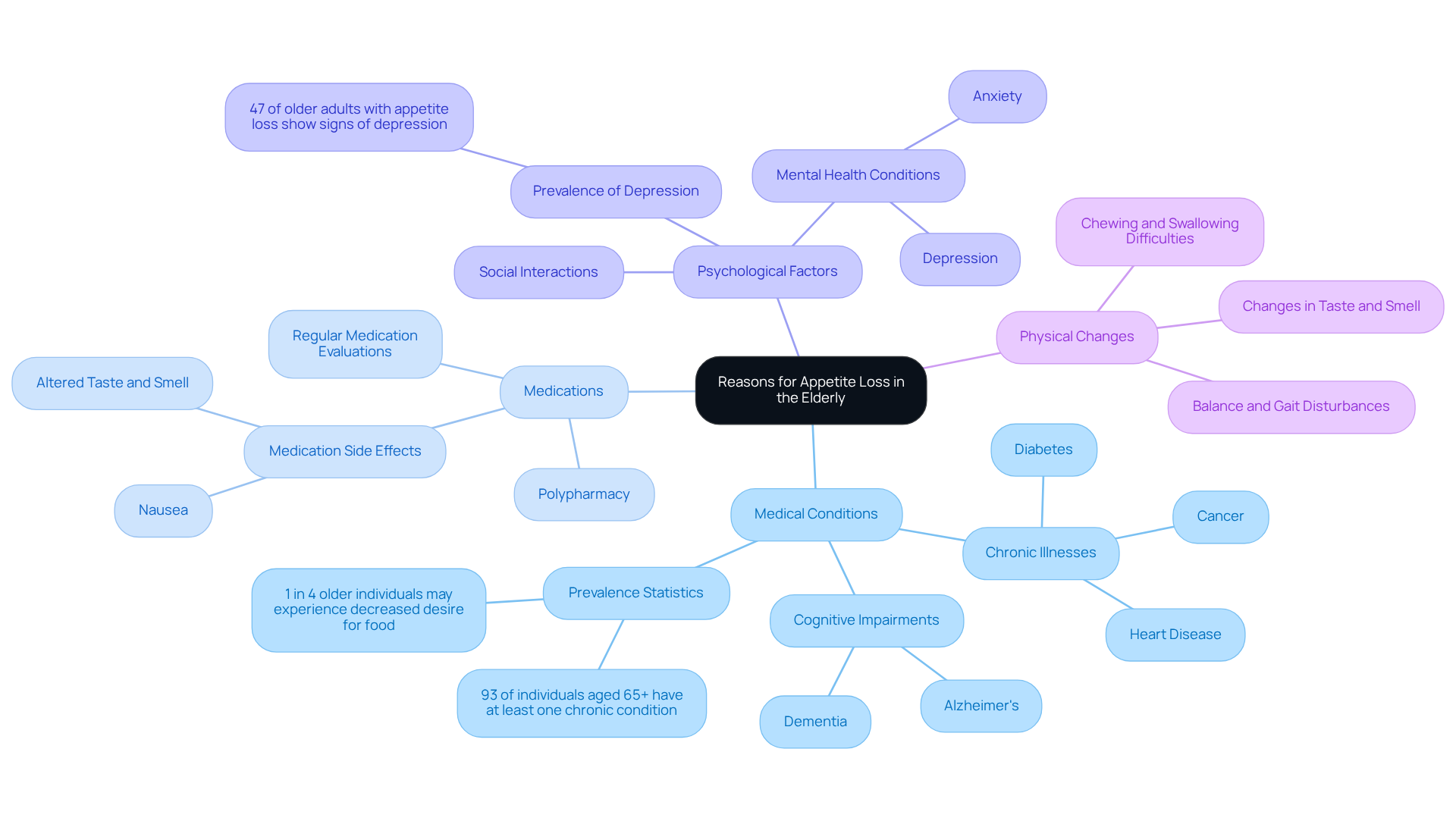
To effectively address the reduced desire for food in an elderly person not eating or drinking, it’s essential to understand the underlying reasons for their diminished interest in nourishment and beverages. This can be a challenging experience for caregivers, who often feel the weight of their loved ones’ struggles. Common causes include:
-
Medical Conditions: Chronic illnesses like diabetes, cancer, and heart disease can significantly impact appetite. It’s concerning to note that nearly 93% of individuals aged 65 and above have at least one long-term condition, often leading to a decrease in their desire for food. Cognitive impairments associated with conditions such as dementia or Alzheimer’s can further complicate nutritional intake. Alarmingly, 1 in 4 older individuals may experience decreased desire for food before malnutrition sets in.
-
Medications: Certain medications can have side effects that diminish hunger. A study found that older adults experiencing a loss of desire for food often had a higher prevalence of polypharmacy, complicating their nutritional status. Regular medication evaluations by healthcare professionals are crucial to identify any prescriptions that might contribute to this issue.
-
Psychological Factors: Mental health conditions, including depression and anxiety, can significantly reduce the desire to eat. About 47% of older adults facing a loss of appetite also show signs of geriatric depression. Social interactions and emotional well-being play a vital role in stimulating appetite, making it essential for caregivers to create a supportive environment. Regular evaluations for depression and other wellness indicators are important for understanding these psychological factors.
-
Physical Changes: Aging often brings changes in taste and smell, which can affect preferences and enjoyment of food. Additionally, difficulties in chewing or swallowing, often worsened by oral health issues, can make eating less enjoyable. Caregivers should monitor subtle signs of an elderly person not eating or drinking, like untouched meal trays. Furthermore, an elderly person not eating or drinking may exhibit balance and gait disturbances, highlighting the need for caregivers to stay vigilant.
By assessing these factors, caregivers can gain a deeper understanding of the specific challenges faced by elderly individuals. This knowledge allows for a more targeted approach to encourage eating and drinking, fostering a nurturing environment that supports their loved ones’ well-being.
Implement Strategies to Stimulate Appetite
To effectively stimulate appetite in elderly individuals, it’s important to consider some thoughtful strategies:
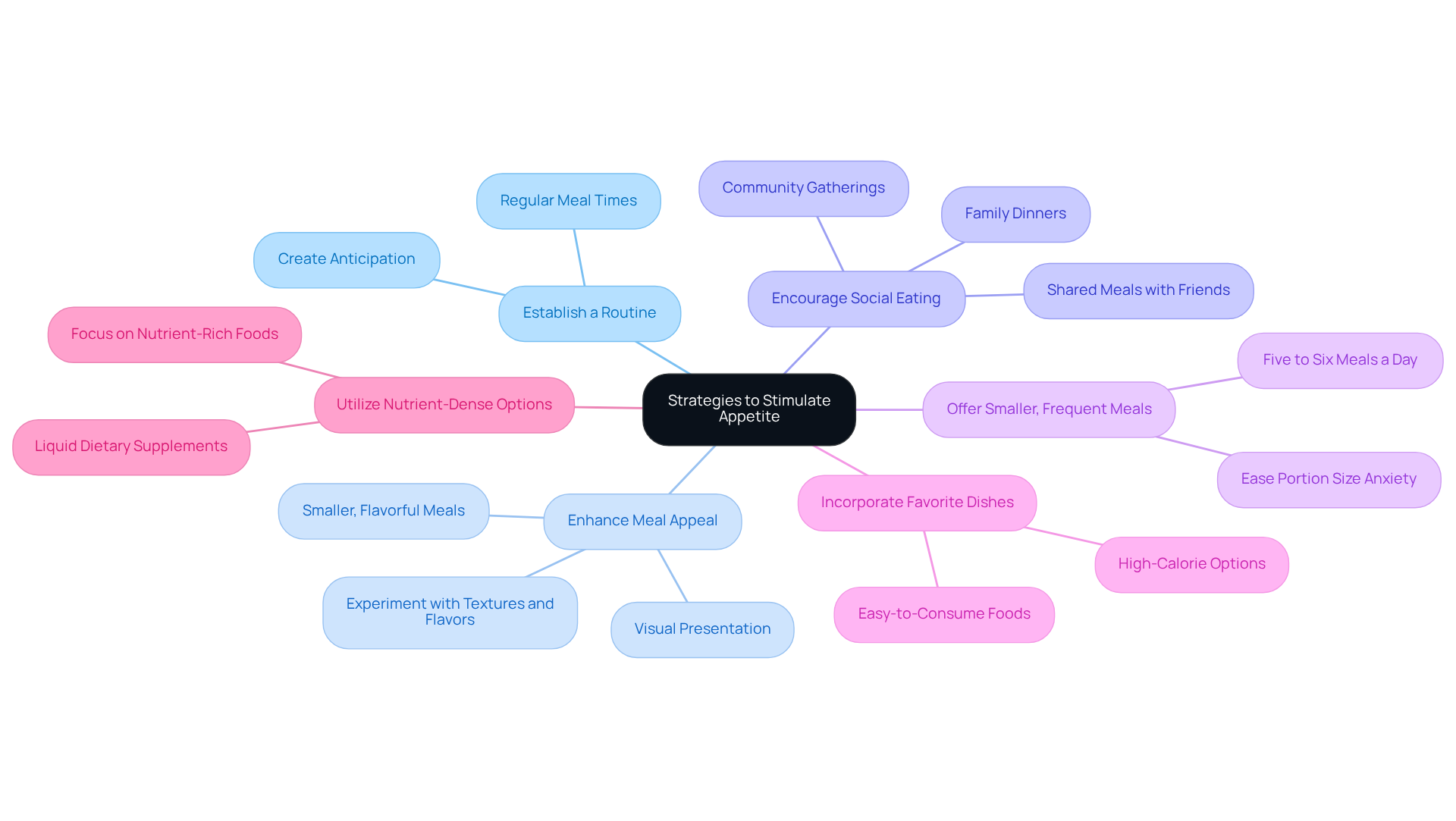
- Establish a Routine: Regular meal times can create a sense of anticipation and normalcy, encouraging seniors to participate in meals. Consistency is key; it helps them feel secure and engaged in their eating habits.
- Enhance Meal Appeal: Making meals visually enticing with colorful plates and garnishes can spark interest. Experimenting with different textures and flavors can significantly enhance the dining experience. Research shows that older adults often eat better when meals are smaller and flavorful, complemented by healthy snacks.
- Encourage Social Eating: Sharing meals with family or friends can greatly enhance the dining experience. Organizing family dinners or inviting friends over fosters social connections, which are crucial for improving appetite and overall well-being. Studies indicate that social eating not only boosts morale but also contributes to better cognitive function and mental health in seniors. Community gatherings, like holiday potlucks, offer wonderful opportunities for seniors to connect while enjoying a variety of dishes.
- Offer Smaller, Frequent Meals: Instead of three large meals, consider providing smaller, more frequent meals throughout the day. This approach can ease the burden of large portions and may lead to increased consumption, especially for those who feel full quickly. In fact, about 1 in 3 seniors in Canada struggles to meet their nutritional needs, emphasizing the critical issue of the elderly person not eating or drinking.
- Incorporate Favorite Dishes: Including preferred items that are easy to consume can rekindle interest in meals. Offering high-calorie, nutrient-dense options like smoothies, yogurt, and soups ensures that seniors receive essential nutrients without overwhelming them with large portions.
- Utilize Nutrient-Dense Options: Focus on foods that are rich in nutrients yet low in volume. This strategy helps meet nutritional requirements without requiring seniors to eat large amounts, which can be daunting. Caregivers should also be aware that certain medications can alter taste and hunger, impacting overall food consumption.
By implementing these compassionate strategies, caregivers can create a more inviting and supportive eating environment for an elderly person not eating or drinking. This not only encourages elderly individuals to consume adequate nutrition but also enhances their overall quality of life.
Monitor Health and Seek Professional Guidance
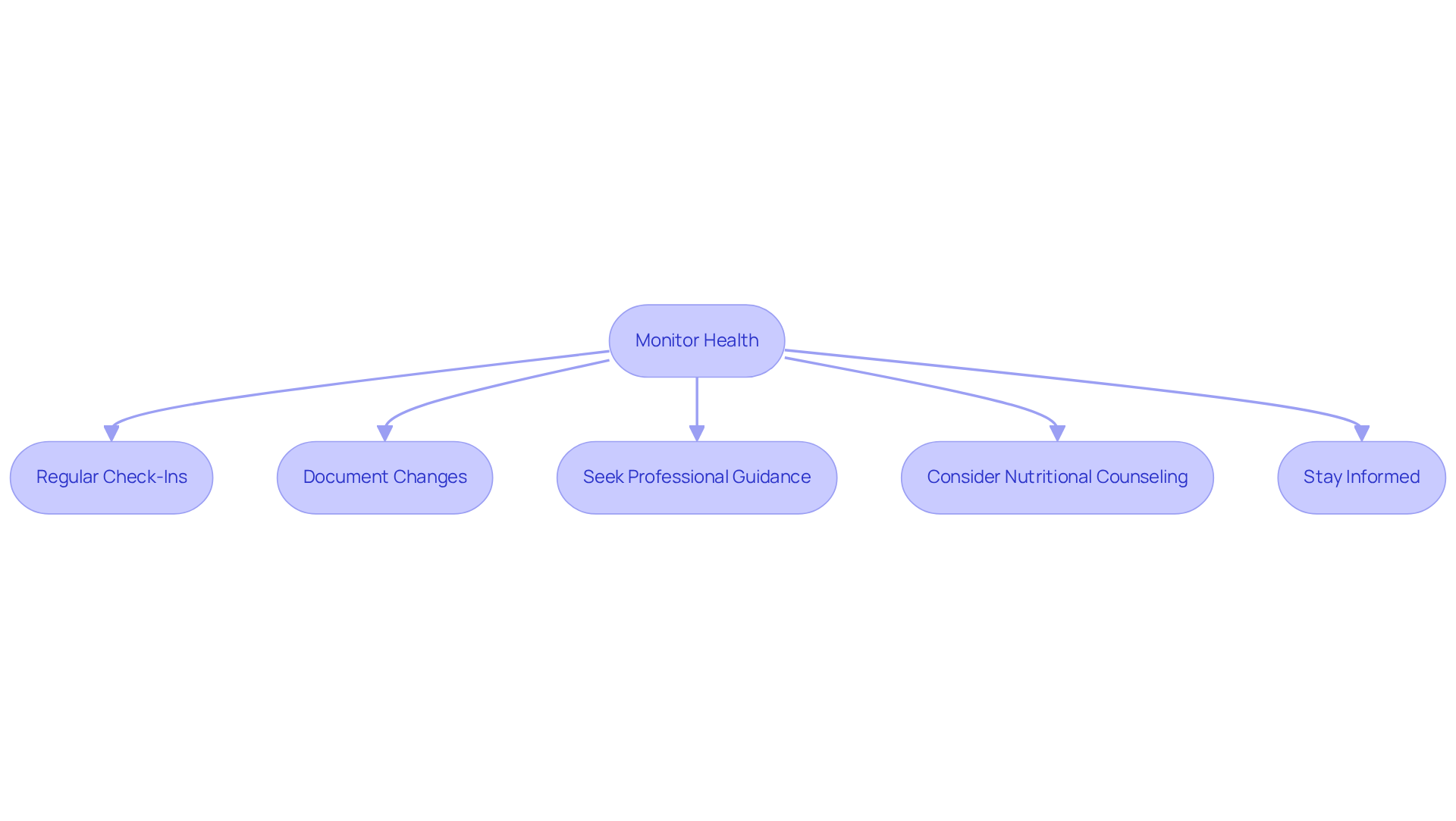
Caring for senior citizens is vital for their nutritional well-being, particularly when there is an elderly person not eating or drinking. It’s important to recognize the emotional challenges caregivers face in this situation. Here are some key steps to help you provide effective oversight:
- Regular Check-Ins: Make it a habit to assess eating habits, weight changes, and overall health regularly. This proactive approach can help you spot concerning trends early. Studies show that one in four older adults experiences a decline in food intake, which can lead to an elderly person not eating or drinking before malnutrition sets in, and up to one-third of seniors may face this issue.
- Document Changes: Keep a detailed log of food and fluid intake, noting any significant shifts in appetite or weight. This record is invaluable for healthcare providers, allowing them to make informed decisions about care. By consistently monitoring, you can identify emerging nutritional concerns promptly. Remember, around 20% of adults aged 65 and older may face mental health conditions that can affect their eating habits.
- If you notice an elderly person not eating or drinking or a persistent or worsening decrease in appetite, don’t hesitate to seek advice from healthcare professionals. Dr. Naushira Pandya emphasizes the importance of medical assessments for weight loss or reduced hunger, especially if accompanied by symptoms like weakness or increased falls. Regular check-ups are crucial; they provide an opportunity to discuss emotional wellness and ensure any changes in condition are addressed quickly.
- Consider Nutritional Counseling: Engaging a registered dietitian can provide personalized advice on meal planning and nutrition, catering to specific dietary needs and preferences. This tailored approach is especially beneficial for seniors with chronic conditions that complicate their nutritional intake.
- Stay Informed: Keep yourself updated on the latest research and guidelines regarding elderly nutrition and appetite management. This knowledge empowers you to make informed decisions, ultimately enhancing the quality of care you provide.
By actively monitoring health and seeking professional guidance, you can ensure that elderly individuals receive the support they need to maintain their nutritional health. This not only improves their well-being but also enriches their quality of life.
Conclusion
Understanding why an elderly person might hesitate to eat or drink is vital for caregivers who want to enhance their loved ones’ nutritional health. By recognizing factors like medical conditions, medication side effects, psychological hurdles, and physical changes, caregivers can adapt their approach to fit each individual’s unique needs. This awareness sets the stage for effective strategies that can spark appetite and improve the overall quality of life for seniors.
Caregivers can take several practical steps to encourage better eating habits:
- Establishing a routine
- Making meals more appealing
- Promoting social eating
- Offering smaller and more frequent meals
- Incorporating favorite dishes
- Choosing nutrient-dense options
These are all effective ways to rekindle interest in food and hydration. Plus, keeping an eye on health and seeking professional advice are crucial to address any underlying issues quickly, helping to prevent further complications.
Ultimately, the well-being of elderly individuals relies heavily on the support they receive from caregivers. By being proactive, compassionate, and well-informed, caregivers can truly make a difference in the nutritional health of seniors. This not only helps combat the risks linked to malnutrition and dehydration but also enriches the emotional and social aspects of their lives. It highlights the importance of holistic care in our aging population.
Frequently Asked Questions
What are the common reasons for appetite loss in the elderly?
Common reasons for appetite loss in the elderly include medical conditions, medications, psychological factors, and physical changes.
How do medical conditions affect appetite in older adults?
Chronic illnesses such as diabetes, cancer, and heart disease can significantly impact appetite. Nearly 93% of individuals aged 65 and above have at least one long-term condition, which can lead to decreased desire for food. Cognitive impairments from conditions like dementia or Alzheimer’s can also complicate nutritional intake.
What role do medications play in appetite loss among the elderly?
Certain medications can have side effects that diminish hunger. Older adults often experience a higher prevalence of polypharmacy, which complicates their nutritional status. Regular medication evaluations by healthcare professionals are essential to identify any prescriptions contributing to appetite loss.
How do psychological factors influence appetite in older adults?
Mental health conditions, such as depression and anxiety, can significantly reduce the desire to eat. About 47% of older adults with a loss of appetite also show signs of geriatric depression, highlighting the importance of social interactions and emotional well-being in stimulating appetite.
What physical changes can affect an elderly person’s appetite?
Aging can bring changes in taste and smell, affecting food preferences and enjoyment. Additionally, difficulties in chewing or swallowing, often due to oral health issues, can make eating less enjoyable. Caregivers should monitor for signs of reduced food intake, such as untouched meal trays.
Why is it important for caregivers to understand the reasons behind appetite loss?
Understanding the reasons behind appetite loss allows caregivers to address specific challenges faced by elderly individuals. This knowledge enables a more targeted approach to encourage eating and drinking, fostering a supportive environment for their loved ones’ well-being.