Introduction
Sundowning presents a significant challenge in dementia care, often leading to heightened confusion and agitation in individuals during the late afternoon and evening. This issue is particularly common among those with Alzheimer’s disease, disrupting not only their lives but also placing considerable emotional strain on caregivers.
Understanding the triggers and symptoms of sundowning is crucial for caregivers. By identifying these factors, they can develop effective strategies to lessen its impact, ultimately improving the quality of life for both patients and their families.
So, what specific interventions can caregivers implement to tackle this complex issue? Here are some actionable tips:
- Establish a Routine: Consistency can help reduce anxiety and confusion.
- Create a Calm Environment: Dimming lights and minimizing noise can promote relaxation.
- Engage in Evening Activities: Gentle activities, such as reading or listening to music, can provide comfort.
- Monitor Diet: Avoiding caffeine and heavy meals in the evening may help ease agitation.
By employing these strategies, caregivers can foster a more peaceful evening routine, enhancing the overall well-being of those they care for.
Define Sundowning and Its Impact on Dementia
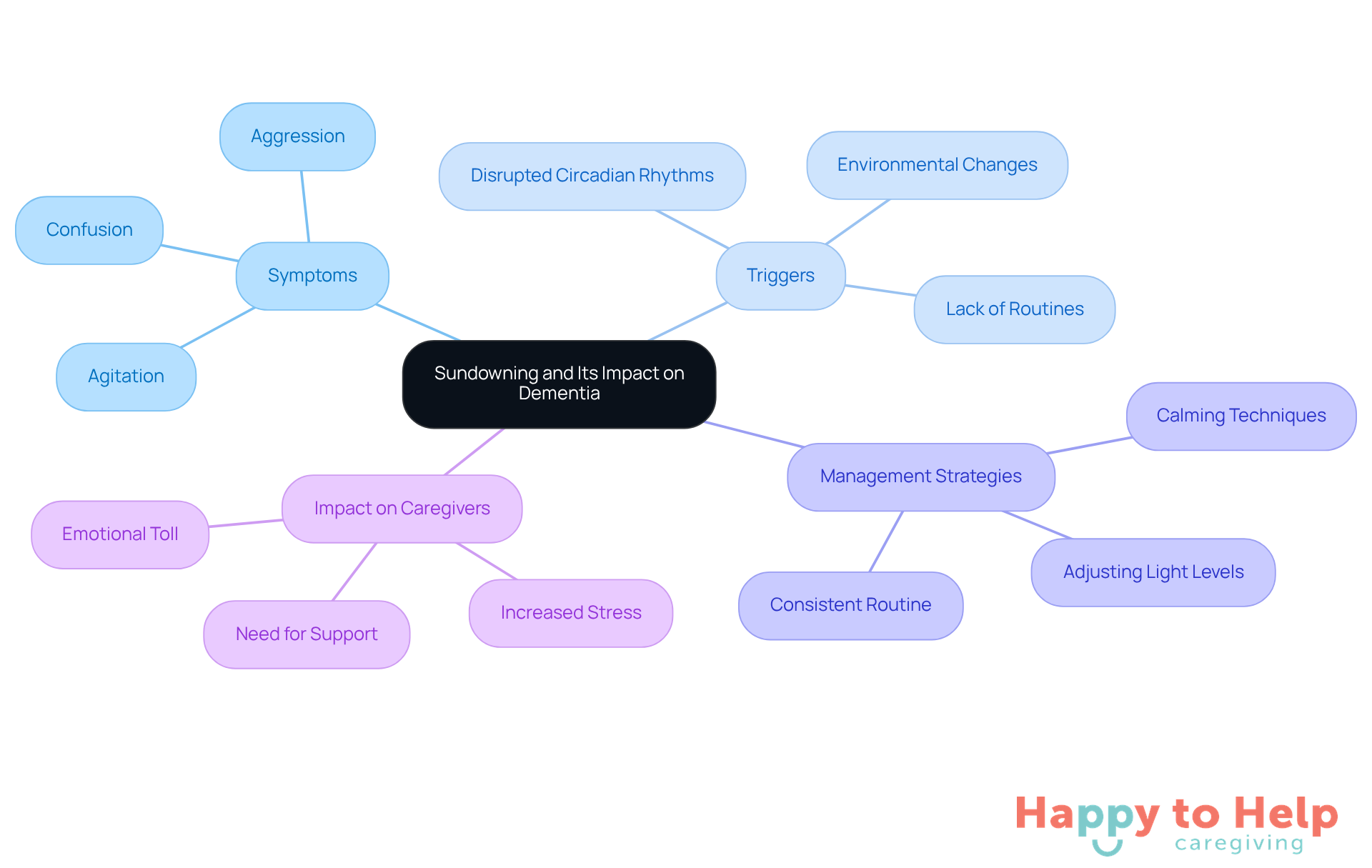
Sundowning presents a significant challenge for caregivers, as individuals with cognitive decline often experience increased confusion, agitation, and behavioral changes in the late afternoon and evening. This phenomenon is particularly common among those with Alzheimer’s disease, leading to restlessness, irritability, and even aggression. For caregivers, understanding what triggers sundowning is crucial, as it can greatly impact the quality of life for both the individual and their family. Recognizing the signs early allows for timely interventions that can help reduce distress and enhance care strategies.
Research shows that approximately 48.9% of individuals with dementia experience evening confusion, underscoring the need for effective management strategies. Disrupted circadian rhythms, lack of routines, and environmental changes are factors that contribute to what triggers sundowning and can worsen symptoms. To combat this, maintaining a consistent daily routine and adjusting light levels can be beneficial. Caregivers should be vigilant in spotting early signs of what triggers sundowning, as taking prompt action can alleviate agitation and improve overall care.
The emotional toll on caregivers is significant, often leading to increased stress and anxiety when managing challenging behaviors. As noted by Diaz, caregivers may witness patients wandering at night, which can be distressing. Employing calming techniques and providing reassurance can foster a more supportive environment. This approach not only aids the individual experiencing evening confusion but also enhances the overall caregiving experience, promoting a sense of security and comfort.
Recent studies highlight the importance of personalized care plans that consider what triggers sundowning and individual preferences. Engaging patients in soothing activities, such as listening to calming music or taking walks, can effectively reduce agitation. Additionally, understanding how medications may influence evening confusion symptoms is vital; some drugs can exacerbate agitation, necessitating a review of prescribed treatments.
In conclusion, addressing sundowning is essential for improving the quality of life for individuals with memory impairment and their caregivers. By implementing effective management strategies and fostering open communication, families can navigate the complexities of cognitive impairment care with greater confidence and compassion.
Identify Factors That Trigger Sundowning
Sundowning symptoms in individuals with dementia present significant challenges for caregivers. As the day progresses, factors such as fatigue, environmental changes, unmet needs, overstimulation, and routine disruptions can exacerbate confusion and agitation.
-
Fatigue is a major contributor. As tiredness sets in, confusion can increase, making it essential for caregivers to monitor energy levels and encourage rest throughout the day. Caregiver fatigue can also play a role, underscoring the importance of self-care for those providing support.
-
Environmental changes can create disorientation. Dimming light and shadows may confuse individuals, while inconsistent indoor lighting and reflective surfaces can worsen the situation. Maintaining consistent lighting and minimizing reflective surfaces can help reduce disorientation.
-
Unmet needs such as hunger, thirst, or discomfort can heighten anxiety and agitation. Caregivers should ensure these basic needs are met promptly to alleviate distress.
-
Overstimulation from a noisy or busy environment can overwhelm individuals, leading to increased agitation. Creating a calm and quiet space during the evening hours can help mitigate these effects.
-
Routine disruptions can unsettle individuals, making them feel insecure. Establishing a consistent routine for activities like meals and bedtime fosters a sense of stability.
By identifying what triggers sundowning and responding to these triggers, caregivers can take proactive steps to reduce their effects, ultimately improving the welfare of those experiencing evening confusion. According to the Alzheimer’s Society, evening confusion can occur at any phase of cognitive decline but is more frequent during the middle and later phases, impacting 2.5% to 66% of individuals with memory disorders. Effectively understanding and managing what triggers sundowning is crucial for enhancing care.
Implement Strategies to Manage Sundowning
Understanding what triggers sundowning is essential, as it can be a challenging issue for caregivers, leading to increased confusion and agitation in individuals with dementia. This phenomenon often occurs in the late afternoon or evening, creating a stressful environment for both the caregiver and the individual. Understanding what triggers sundowning is crucial for effectively managing it and improving the quality of life for everyone involved.
To tackle this issue, caregivers can implement several key strategies:
- Establish a Routine: Maintaining a consistent daily schedule fosters a sense of security and predictability, which is crucial for individuals with dementia. Research indicates that structured routines can significantly reduce confusion and anxiety, leading to improved overall well-being.
- Create a Calm Environment: Soft lighting and reduced noise levels in the evening can create a soothing atmosphere. This approach helps mitigate agitation and confusion, making the home more conducive to relaxation.
- Promote Daylight Exposure: Ensuring ample natural light during the day aids in regulating circadian rhythms, which can reduce evening confusion symptoms. Exposure to bright light has been shown to positively impact mood and behavior in dementia patients.
- Participate in Low-Stimulation Activities: Activities like reading, enjoying soothing music, or browsing through photo albums can assist in calming people experiencing evening confusion. These gentle engagements provide comfort and distraction from distressing thoughts or feelings.
- Monitor Physical Needs: Regularly checking for hunger, thirst, or discomfort is essential. Addressing these physical needs promptly can prevent unnecessary agitation and contribute to a more peaceful evening routine.
By employing these strategies, caregivers can significantly reduce the frequency and intensity of sundowning episodes by understanding what triggers sundowning, leading to a calmer and more manageable evening for both the caregiver and the individual.
Conclusion
Sundowning poses a significant challenge in dementia care, impacting both individuals with cognitive decline and their caregivers. The confusion, agitation, and behavioral changes that often arise during late afternoons and evenings can be overwhelming. Understanding the triggers and effective management strategies is crucial for caregivers to enhance the quality of life for those they support.
To mitigate the effects of sundowning, establishing consistent routines and creating calming environments are essential. Factors like fatigue, environmental changes, and overstimulation can worsen confusion. Personalized care plans and soothing activities can provide comfort and security, helping to reduce the frequency and intensity of sundowning episodes.
Addressing sundowning goes beyond merely managing symptoms; it involves fostering a compassionate caregiving environment where individuals with dementia feel safe and understood. Caregivers should also prioritize their own well-being, ensuring they are equipped to handle the complexities of cognitive impairment. By embracing effective interventions, caregivers can transform their experience, leading to more peaceful evenings and improved overall well-being for everyone involved.
Frequently Asked Questions
What is sundowning?
Sundowning is a phenomenon where individuals with cognitive decline, particularly those with dementia, experience increased confusion, agitation, and behavioral changes during the late afternoon and evening.
Who is most affected by sundowning?
Sundowning is particularly common among individuals with Alzheimer’s disease, leading to symptoms such as restlessness, irritability, and aggression.
What triggers sundowning in individuals with dementia?
Factors that contribute to sundowning include disrupted circadian rhythms, lack of routines, and environmental changes.
How prevalent is sundowning among individuals with dementia?
Research indicates that approximately 48.9% of individuals with dementia experience evening confusion.
What strategies can caregivers use to manage sundowning?
Caregivers can manage sundowning by maintaining a consistent daily routine, adjusting light levels, and recognizing early signs of agitation to take timely action.
What is the emotional impact of sundowning on caregivers?
Caregivers often experience significant emotional toll, including increased stress and anxiety, when managing the challenging behaviors associated with sundowning.
What techniques can help create a supportive environment for individuals experiencing sundowning?
Employing calming techniques, providing reassurance, and engaging individuals in soothing activities, such as listening to calming music or taking walks, can foster a more supportive environment.
How can medications influence sundowning symptoms?
Some medications may exacerbate agitation and evening confusion symptoms, making it important for caregivers to review prescribed treatments.
Why is it important to address sundowning?
Addressing sundowning is essential for improving the quality of life for individuals with memory impairment and their caregivers, enabling better management of cognitive impairment care.
List of Sources
- Define Sundowning and Its Impact on Dementia
- What is Sundowning? Causes & Coping Strategies | alz.org (https://alz.org/help-support/caregiving/stages-behaviors/sleep-issues-sundowning)
- sundowning treatment gibbs | UCI Health | Orange County, CA (https://ucihealth.org/about-us/news/2023/04/sundowning-treatment-gibbs)
- The 1 Dementia Symptom We Don’t Talk About Enough (https://huffpost.com/entry/sundowning-is-the-dementia-symptom-we-dont-talk-about-enough-g_l_691f838ce4b047290e295f4b)
- Sundowning: the condition with symptoms that appear at sunset (https://dementiasplatform.uk/news-and-media/blog/sundowning-the-condition-with-symptoms-that-appear-at-sunset)
- Sundowning Syndrome in Dementia: Mechanisms, Diagnosis, and Treatment – PMC (https://pmc.ncbi.nlm.nih.gov/articles/PMC11856004)
- Identify Factors That Trigger Sundowning
- Sundowning and dementia (https://alzheimers.org.uk/about-dementia/stages-and-symptoms/dementia-symptoms/sundowning)
- Evening phenomenon could be warning sign of dementia (https://getsurrey.co.uk/news/health/distressing-evening-phenomenon-could-warning-32877338)
- Sundowning: the condition with symptoms that appear at sunset (https://dementiasplatform.uk/news-and-media/blog/sundowning-the-condition-with-symptoms-that-appear-at-sunset)
- Sundowning Syndrome in Dementia: Mechanisms, Diagnosis, and Treatment – PMC (https://pmc.ncbi.nlm.nih.gov/articles/PMC11856004)
- Frontiers | Sundowning in Dementia: Clinical Relevance, Pathophysiological Determinants, and Therapeutic Approaches (https://frontiersin.org/journals/medicine/articles/10.3389/fmed.2016.00073/full)
- Implement Strategies to Manage Sundowning
- Coping With Agitation, Aggression, and Sundowning in Alzheimer’s Disease (https://nia.nih.gov/health/alzheimers-changes-behavior-and-communication/coping-agitation-aggression-and-sundowning)
- Sundowning: What to know if your loved one with dementia experiences late-day symptoms – Harvard Health (https://health.harvard.edu/mind-and-mood/sundowning-what-to-know-if-your-loved-one-with-dementia-experiences-late-day-symptoms)
- Tips for Managing Sundowning (https://brightfocus.org/resource/tips-for-managing-sundowning)
- Clock changes and dementia: Tips for managing the challenge (https://deseret.com/family/2025/10/29/time-change-alzheimers-dementia-patients-caregivers-struggle-sundowning)
- Sundowning Strategies for Family Caregivers – Sycamore Creek Ranch (https://scrmemorycare.com/sundowning-strategies-for-family-caregivers)