Overview
Caring for someone with end-stage dementia can be incredibly challenging, especially when hallucinations come into play. It’s essential to recognize these moments not just as symptoms, but as emotional experiences that can deeply affect both the individual and their caregiver. Caregivers often feel overwhelmed, stressed, and even burnt out. It’s okay to acknowledge these feelings; they are valid and shared by many in similar situations.
To effectively manage hallucinations, caregivers can employ calming communication strategies. Speaking softly and reassuringly can help ease the individual’s distress. Additionally, making small adjustments to the environment—like reducing noise or providing familiar objects—can create a sense of comfort and safety. These practical steps can make a significant difference in the daily lives of both caregivers and those they care for.
However, amidst these challenges, it’s crucial for caregivers to prioritize their own well-being. Taking time for self-care isn’t just a luxury; it’s a necessity. Engaging in activities that bring joy and relaxation can help replenish the emotional reserves needed to provide compassionate care.
Remember, you’re not alone in this journey. Many caregivers have walked this path and found ways to cope and thrive. Sharing stories and experiences can foster a sense of community and support. As one caregiver shared, “Finding moments of peace amidst the chaos has been my saving grace.”
In the face of these challenges, it’s important to hold onto hope and seek support. By recognizing the emotional weight of caregiving and implementing practical strategies, you can navigate this journey with compassion and resilience.
Introduction
End-stage dementia poses a significant challenge, not just for those diagnosed but also for the caregivers who stand by them. As cognitive functions decline, individuals often face distressing symptoms like severe memory loss and unsettling hallucinations. These experiences can complicate daily interactions and care, leaving caregivers feeling overwhelmed.
This guide is here to support caregivers with essential strategies and insights to manage these hallucinations effectively. Our goal is to foster a sense of safety and comfort for your loved ones. How can caregivers navigate the emotional turmoil and practical difficulties that arise in these critical moments? It’s vital to ensure both your well-being and that of the person you care for.
You’re not alone in this journey. Many caregivers share similar feelings of stress and burnout. By understanding these challenges and exploring practical solutions, we can work together to create a nurturing environment for everyone involved. Remember, it’s okay to seek help and lean on others for support.
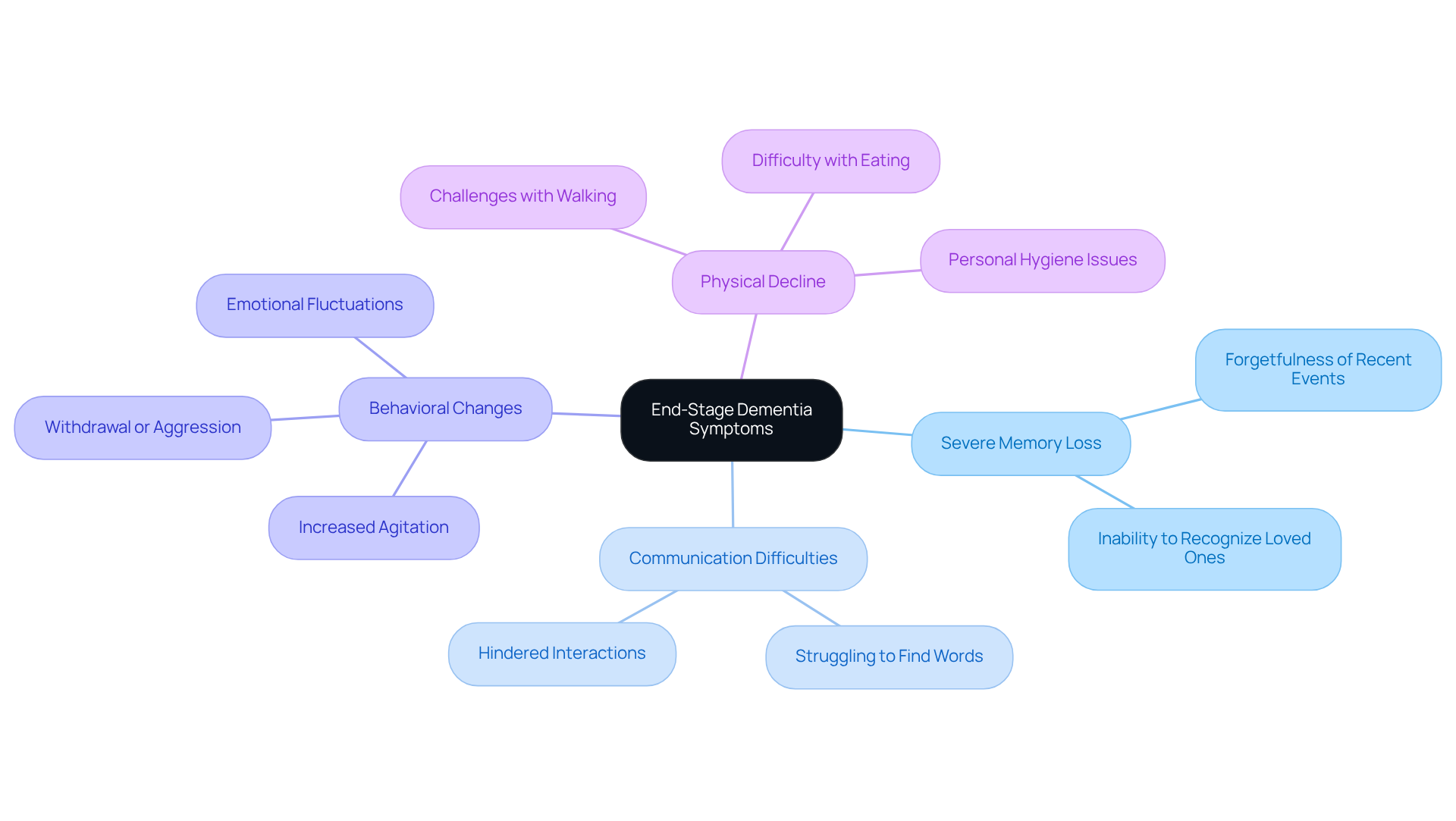
Understand End-Stage Dementia and Its Symptoms
End-stage cognitive impairment brings significant cognitive decline, often leaving individuals unable to communicate effectively, recognize loved ones, or carry out daily activities. Common symptoms include severe memory loss, confusion, difficulty with motor skills, and changes in behavior. Caregivers should be mindful that emotional fluctuations, such as anxiety and depression, may also arise. Understanding these symptoms helps caregivers prepare for the emotional and physical challenges of supporting their loved ones, allowing them to provide compassionate and informed assistance.
Key Symptoms to Recognize:
- Severe Memory Loss: Forgetting recent events or familiar faces can lead to distress for both the individual and their caregivers.
- Communication Difficulties: Struggling to find words or express thoughts can hinder interactions, making connection feel challenging.
- Behavioral Changes: Increased agitation, withdrawal, or aggression may occur, requiring patience and understanding. Notably, 76% of individuals with Alzheimer’s disease experience agitation, highlighting the emotional difficulties caregivers may face.
- Physical Decline: Challenges with walking, eating, or personal hygiene can significantly impact daily life.
Recognizing these symptoms allows caregivers to anticipate the needs of their loved ones, fostering a nurturing atmosphere that prioritizes comfort and dignity. As care specialists emphasize, maintaining a compassionate approach is vital; individuals in this stage can still benefit from interaction, even if they cannot initiate it themselves. This understanding helps caregivers forge meaningful connections, despite the challenges posed by the disease.
With projections indicating that the number of individuals with Alzheimer’s disease could reach 13.8 million by 2060, recognizing these symptoms and providing effective support is more crucial than ever. Integrating insights from memory care experts can further enhance caregivers’ ability to navigate this difficult journey.
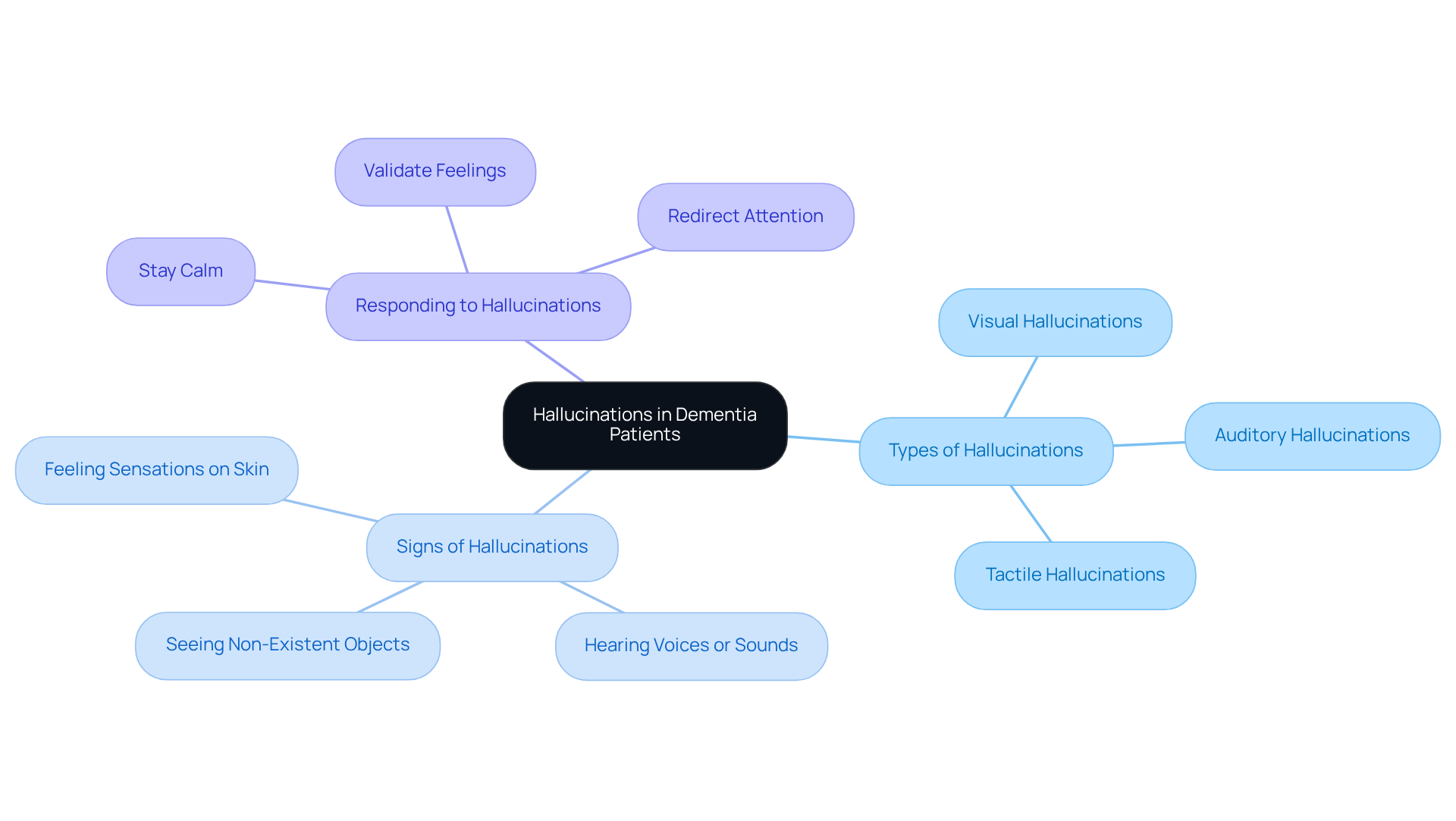
Recognize Hallucinations in Dementia Patients
Hallucinations, including end-stage dementia hallucinations, in individuals with cognitive decline can take many forms, such as visual, auditory, or tactile experiences. Imagine a patient who sees people or objects that aren’t there, hears voices, or feels sensations that simply don’t exist. Recognizing end-stage dementia hallucinations is crucial for caregivers, as it enables them to respond appropriately and provide comfort. Notably, visual distortions are the most common type encountered in patients experiencing end-stage dementia hallucinations, especially in advanced Alzheimer’s disease, where up to 50 percent of individuals may exhibit such symptoms.
Signs of Hallucinations:
- Visual Hallucinations: Patients might describe seeing animals, people, or objects that aren’t present. This type is particularly common in Lewy body dementia, often associated with end-stage dementia hallucinations.
- Auditory Hallucinations: Patients in advanced stages may hear voices or sounds that others cannot, which can be distressing and lead to confusion.
- Tactile Hallucinations: Some patients with end-stage dementia might feel sensations on their skin, like bugs crawling, which can be quite alarming.
Responding to Hallucinations:
- Stay Calm: Approach the situation with a calm demeanor. This can help prevent escalating the patient’s anxiety. Your steady presence can be a source of comfort.
- Validate Feelings: Acknowledge the patient’s experience without disputing their perception. As Dr. Bianca Cavedoni-Urbano suggests, meeting patients in their reality can help ease feelings of fear or confusion.
- Redirect Attention: Gently guide the patient’s focus to a different activity or topic. Engaging them in a familiar task or conversation can be beneficial and soothing.
Additionally, caregivers should consider making physical adjustments to the environment to help alleviate symptoms. This might include removing triggering items or improving lighting. By understanding and acknowledging end-stage dementia hallucinations, caregivers can provide essential support and comfort to their loved ones, thereby nurturing a sense of safety during challenging times.
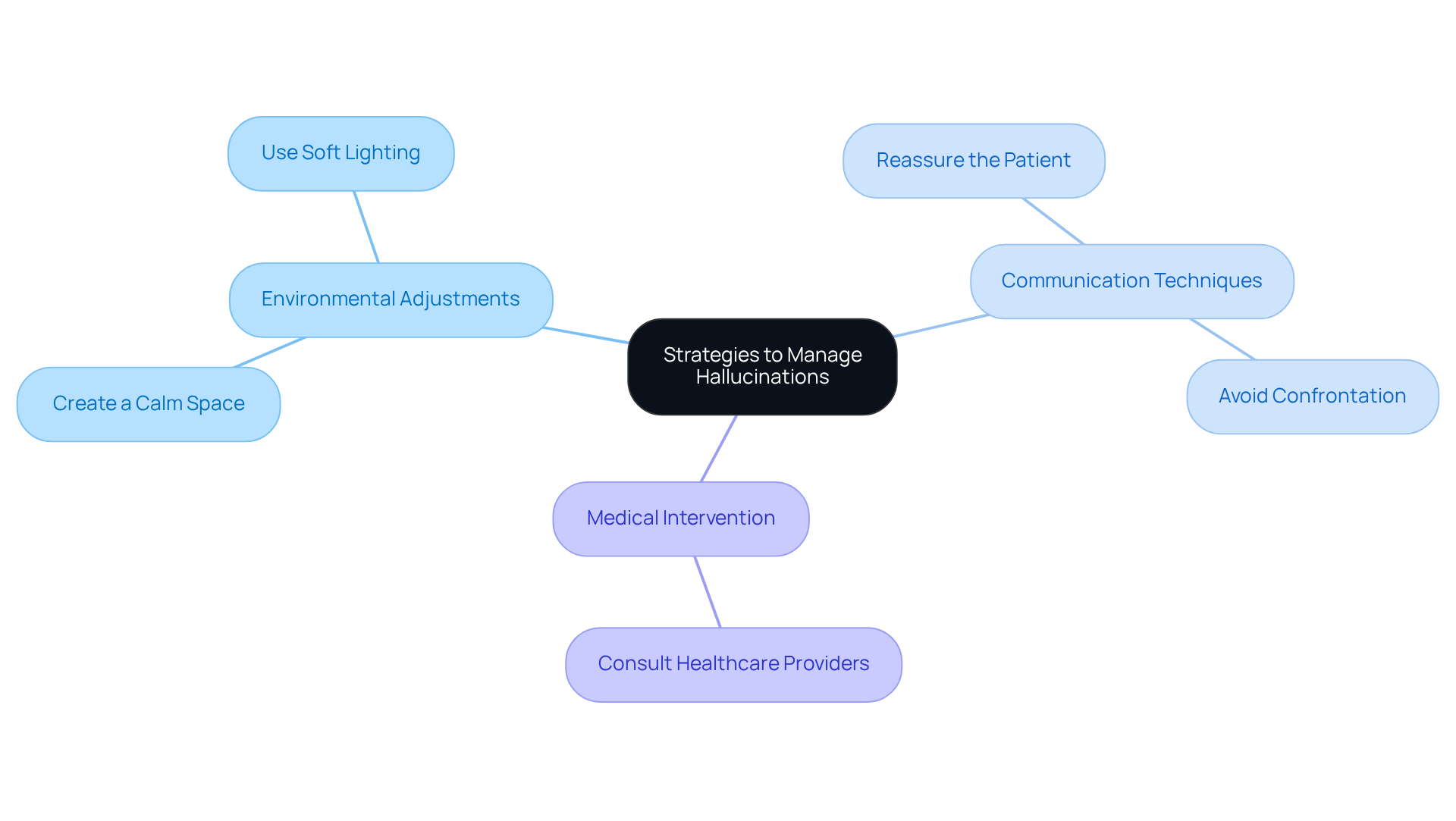
Implement Strategies to Manage Hallucinations
Managing perceptual disturbances, such as end-stage dementia hallucinations, in dementia patients requires a thoughtful blend of environmental adjustments, effective communication techniques, and, when necessary, medical intervention. Caregivers often face emotional challenges, and it’s essential to address these with compassion and understanding. Here are some key strategies that can make a difference:
Environmental Adjustments:
- Create a Calm Space: Reducing noise and clutter can help minimize triggers for hallucinations. A serene environment can significantly ease distress. Establishing a secure and stable home setting is vital in lessening triggers for false perceptions.
- Use Soft Lighting: Harsh lighting can intensify distorted perceptions. Opting for softer, ambient lighting fosters a more comforting atmosphere.
Communication Techniques:
- Reassure the Patient: Using a gentle tone conveys safety and care, helping to ease anxiety. Acknowledge what they see or hear without confirming its reality. This approach validates their feelings without reinforcing the perception.
- Avoid Confrontation: Instead of arguing against the existence of their perceptions, focus on affirming the patient’s emotions. This method builds trust and understanding, allowing for a deeper connection. Remember, caregiver anxiety can easily transfer to the individual, escalating their distress. Maintaining a calm demeanor is essential.
Medical Intervention:
- Consult Healthcare Providers: If hallucinations become frequent or distressing, it’s crucial to consult healthcare professionals for potential medication adjustments or therapeutic options. Discussing any relevant medical issues or medications with the physician is important, as some may lead to false perceptions or delusions.
By applying these strategies, caregivers can greatly improve their experience, alleviating anxiety for both the patient and themselves while fostering a sense of security and comfort. For instance, a patient might report seeing small children playing in the living room when no one else is there, illustrating the nature of hallucinations. By understanding and addressing these experiences, caregivers can offer more effective support.
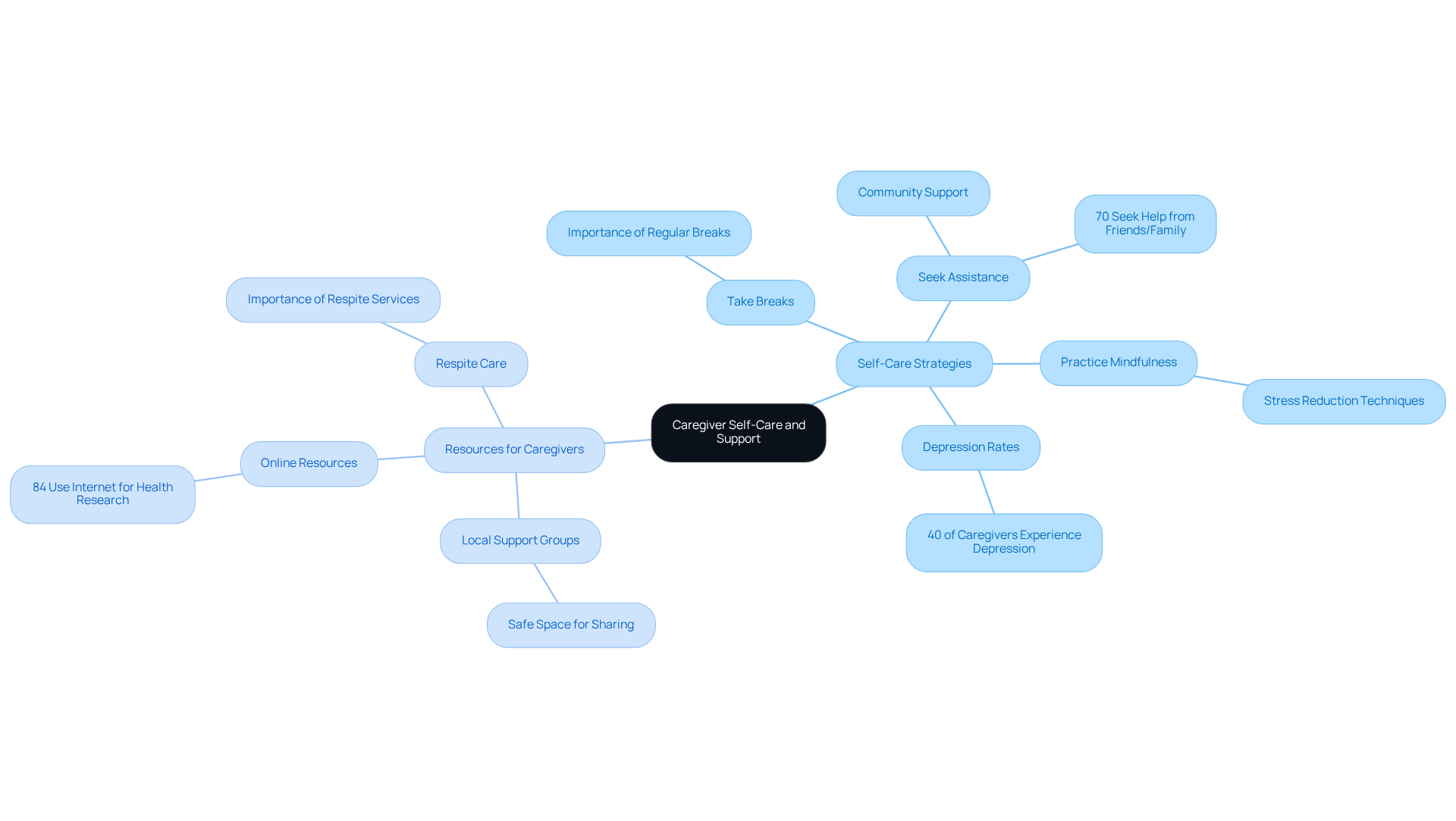
Prioritize Caregiver Self-Care and Support
Caregivers often face immense pressure and emotional challenges while navigating the complexities of cognitive impairment care. It’s crucial for them to focus on self-care to maintain their well-being and effectiveness in their roles. Did you know that around 40% of family supporters of individuals with cognitive impairments experience depression? That’s significantly higher than the 5-17% seen in those who aren’t caregivers.
Self-Care Strategies:
- Take Breaks: Make it a point to schedule regular breaks. Whether it’s a short walk, indulging in a hobby, or spending time with friends, these moments are vital for relieving stress and preventing burnout.
- Seek Assistance: Consider joining support groups or online forums where caregivers can share their experiences and gain insights from others in similar situations. About 70% of caregivers look for information, assistance, or help from friends and family. Additionally, 70% of those caring for individuals with dementia find organizing care to be stressful, underscoring the importance of community support.
- Practice Mindfulness: Engaging in mindfulness or relaxation techniques can significantly reduce stress and enhance emotional resilience. This practice is essential for maintaining mental health in such a demanding caregiving role.
Resources for Caregivers:
- Local Support Groups: Many communities offer support groups for caregivers, providing a safe space to share challenges and solutions. These groups can help alleviate feelings of isolation and offer valuable emotional support.
- Online Resources: Websites and forums dedicated to dementia care can be a treasure trove of information and community support. With 84% of caregivers using the Internet for health-related research, these resources can truly be a lifeline for those seeking guidance.
- Respite Care: Access to respite services is crucial for caregivers, allowing them to take necessary breaks while ensuring their loved ones receive professional assistance. This support can greatly enhance the well-being and efficiency of those providing care.
By prioritizing self-care, caregivers can improve their ability to offer compassionate and effective support, ultimately benefiting both themselves and their loved ones. As highlighted by the Alzheimer’s Association, ensuring caregivers have access to support resources is vital for enhancing their health and the quality of care they provide.
Conclusion
Understanding and managing end-stage dementia, especially the hallucinations that often accompany it, is a vital part of caregiving. This journey can be incredibly challenging, and it’s essential for caregivers to be equipped with the right knowledge and strategies. By recognizing the symptoms of end-stage dementia and the nature of hallucinations, caregivers can offer compassionate support that truly acknowledges the reality of their loved ones’ experiences.
The article highlights the importance of understanding the symptoms of end-stage dementia, such as:
- Severe memory loss
- Communication difficulties
- Behavioral changes
It also emphasizes the significance of recognizing hallucinations, which can take many forms. Caregivers are encouraged to:
- Create a calming environment
- Communicate effectively
- Prioritize their own self-care
This is crucial for maintaining their well-being while providing care.
Ultimately, caregivers play a vital role in navigating the complexities of end-stage dementia. By prioritizing their own mental health and seeking support, they can enhance their ability to provide effective care. This holistic approach not only benefits the loved ones they care for but also fosters a healthier dynamic that can ease the emotional burdens associated with this difficult journey. Embracing these strategies can lead to a more compassionate and supportive caregiving experience, ensuring that both caregivers and patients find moments of peace amidst the challenges of dementia.
Frequently Asked Questions
What is end-stage dementia?
End-stage dementia refers to the final phase of cognitive impairment characterized by significant cognitive decline, where individuals often struggle to communicate, recognize loved ones, or perform daily activities.
What are the common symptoms of end-stage dementia?
Common symptoms include severe memory loss, communication difficulties, behavioral changes, and physical decline, such as challenges with walking, eating, or personal hygiene.
How does severe memory loss manifest in individuals with end-stage dementia?
Severe memory loss may involve forgetting recent events or familiar faces, which can be distressing for both the individual and their caregivers.
What communication difficulties do individuals with end-stage dementia face?
Individuals may struggle to find words or express their thoughts, making it challenging to maintain interactions and connections with others.
What behavioral changes might caregivers observe in individuals with end-stage dementia?
Caregivers may notice increased agitation, withdrawal, or aggression in individuals, which requires patience and understanding.
Why is it important for caregivers to recognize these symptoms?
Recognizing symptoms allows caregivers to anticipate the needs of their loved ones, fostering a nurturing atmosphere that prioritizes comfort and dignity.
How can caregivers maintain meaningful connections with individuals in end-stage dementia?
Caregivers can maintain meaningful connections by providing compassionate interaction, even if the individual cannot initiate it themselves.
What is the projected impact of Alzheimer’s disease by 2060?
Projections indicate that the number of individuals with Alzheimer’s disease could reach 13.8 million by 2060, making it increasingly important to recognize symptoms and provide effective support.
How can insights from memory care experts assist caregivers?
Integrating insights from memory care experts can enhance caregivers’ ability to navigate the challenges of supporting individuals with end-stage dementia.